The most effective management of OA depends on patient behaviors like weight loss, increasing physical activity, and participating in self-management programs. This module describes 4 tools providers can use when counseling patients with OA about behavior change.
DOWNLOAD PDFAdditional Resources: Engaging Patients in OA Management Strategies Presentation with Speaker Guide
This presentation is intended to facilitate peer-to-peer education (e.g., grand rounds, medical school education lecture) among healthcare providers (HCPs) to increase education about osteoarthritis (OA) among HCPs and their patients, specifically to engage patients in self-management strategies to address OA symptoms. Learning objectives for HCPs include:
- Recognize OA as a chronic, serious disease and current symptom management strategies.
- Understand the importance of engaging patients in self-management strategies to help improve OA symptoms.
- Acquire knowledge, skills, and resources to meet patients where they are in terms of behavior change.
- Learn techniques to engage patients in meaningful conversation and shared decision making to promote patient participation in OA self-management
Because every patient with osteoarthritis (OA) is different, you will need to tailor your recommendations often using a multi-modal and individualized approach to address symptoms. The most effective OA treatments depend on patient behaviors like weight loss, increasing physical activity, and participating in self-management programs. Changing long-established behaviors is hard. Most Americans, even those without arthritis, would benefit from changes in their health habits. For example, fewer than one in four Americans meet both the aerobic and muscle-strengthening physical activity guidelines,1 and more than 70% of adults are overweight or obese.2
Primary care clinicians are in a unique position to help patients with OA make behavior changes that will benefit not only their OA symptoms but other chronic conditions as well.
Physical activity is effective for decreasing arthritis pain, increasing physical function, and managing chronic comorbidities. Participation in evidence-based physical activity programs may also reduce healthcare costs nearly $1,000 per person annually.4,5 Nevertheless, 40% of adults do not receive counseling about physical activity.6 Weight loss counseling is a key component of successful weight loss among patients. Adults with arthritis and overweight or obesity who receive provider counseling about weight loss are four times more likely to attempt to lose weight; yet, fewer than half of those adults are actually receiving such counseling.7
We will describe 4 tools you can use when counseling patients with OA about behavior change: Motivational Interviewing, Brief Action Planning, Physical Activity as a Vital Sign, and 5 As. These approaches are not necessarily mutually exclusive.
Motivational Interviewing
Motivational interviewing was first developed for use in addiction counseling. It has since been shown to be effective for chronic disease management and behavior change in multiple diseases.8 In the IMPAACT trial (Improving Motivation for Physical Activity in Arthritis Clinical Trial), Gilbert et al found that patients with knee OA who received motivational interviewing related to physical activity in addition to brief physician counseling experienced improved self-reported function and a small improvement in pain.9
 Providers can use motivational interviewing (MI) to help guide patients—particularly those who feel stuck or are even ambivalent about changing their habits—through the process of setting and making health behavior goals, such as increasing their physical activity level, changing their diet, or participating in a self-management program.
Providers can use motivational interviewing (MI) to help guide patients—particularly those who feel stuck or are even ambivalent about changing their habits—through the process of setting and making health behavior goals, such as increasing their physical activity level, changing their diet, or participating in a self-management program.
Embracing the “spirit” of MI, providers assess patients’ readiness to change and call on patients’ personal motivations, strengths, and experiences. The “Spirit of MI” encourages providers to have conversations with patients that:
- Are “Collaborative”: Providers work with patients as partners rather than directing patients or telling them what they should do. Collaboration is fostered through rapport building.
- Are “Evocative”: Using open-ended questions and reflective listening, providers evoke from the patient what their goals, motivations, and strengths are, drawing out and reflecting back the patient’s own reasons and approaches for behavior change.
- “Honor the patient’s autonomy”: While providers may want patients to make healthy behavior changes, ultimately, it is up to the patient whether or not to act. Empowering the patient to make this decision can actually help enable the behavior change.8
Table: Standard Approach v. Motivational Interviewing Example2
STANDARD APPROACH |
MOTIVATIONAL INTERVIEWING |
COMMENTS |
| As your healthcare professional, I really think that you should exercise on a daily basis. | What are your thoughts about exercising? | Focus is on client’s concerns. |
| There are all kinds of ways you could exercise. You could walk, ride a bike, swim or go to a gym. | What kinds of activities do you enjoy? | Egalitarian partnership. |
| You say that you don’t have time to exercise, but exercise is so important for your joints, you should make time for it. | You say that time is a barrier for you to exercise, what ideas do you have to fit physical activity into your daily routine? | Focus is on client’s concerns. Match intervention to client’s level of motivation. |
| I’ve written some goals for you about increasing your exercise. | Tell me what you would like to work on for the next three months. | Emphasis is on client personal choice. Goals are set collaboratively. |
| You say you want to be more active, yet you don’t do the home exercise program I gave you. This tells me that you just are not interested. | Your ambivalence about exercise is normal. Tell me how you would like to move forward. | Ambivalence is a normal part of the change process. |
Ehrlich-Jones, L., Mallinson, T., Fischer, H., Bateman, J., Semanik, P. A., Spring, B., et.al(2010). Increasing physical activity in patients with arthritis: a tailored health promotion program. Chronic Illness, 6(4), 272–281. https://doi.org/10.1177/1742395309351243. Reprinted by Permission of SAGE Publications, Ltd. |
||
You can start to use some key motivational interviewing questions and concepts in clinic visits right away even while you are working on perfecting your skills! For a thorough explanation and demonstration of motivational interviewing in a primary care setting, including a sample provider-patient conversation about weight loss, refer to this article11: Kathleen G. Reims, MD, FAAFP, and Denise Ernst, PhD “Using Motivational Interviewing to Promote Healthy Weight,” Fam Pract Manag. 2016 Sep-Oct;23(5):32-38. Other resources on motivational interviewing can be found at the end of this module.
Brief Action Planning (BAP)
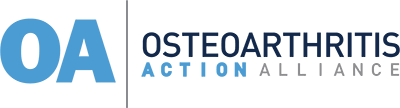
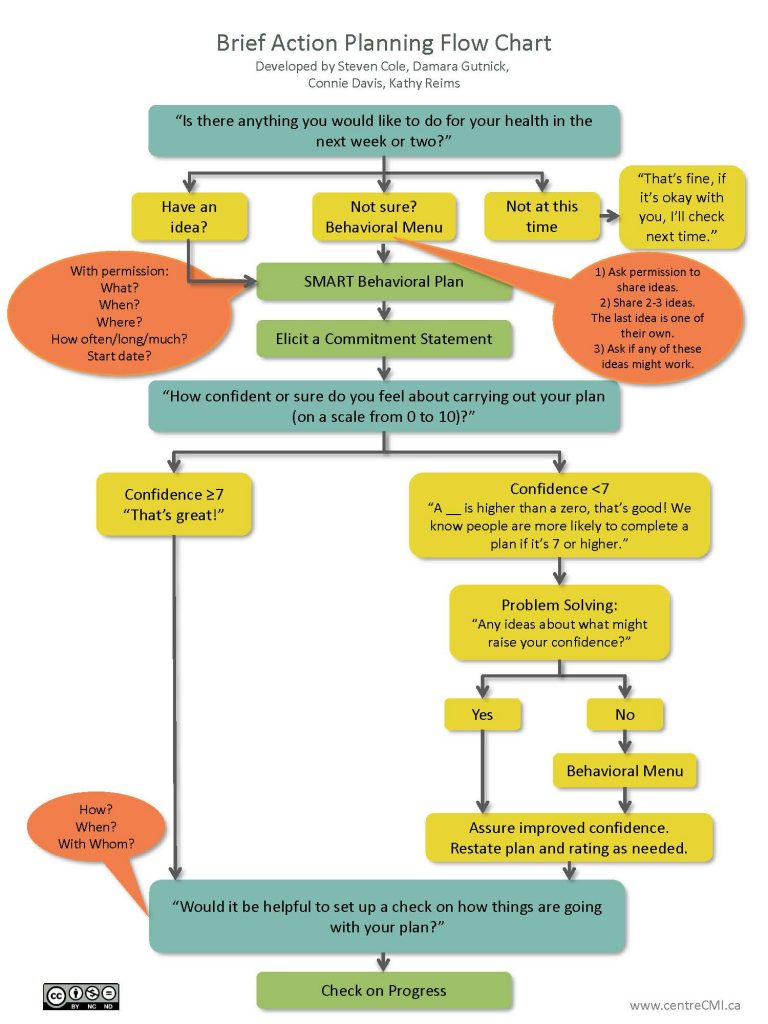
Another model that some clinicians find helpful is Brief Action Planning (BAP). BAP is founded in the concepts of motivational interviewing with particular emphasis on the “spirit of MI” and is easily implemented in primary care settings. Gutnick et al (2014) conclude through their research that “BAP is a useful self-management support technique for busy medical practices to promote health behavior change and build patient self-efficacy for improved long-term clinical outcomes in chronic illness care and disease prevention” (p 17).12
In BAP, patients are assisted in developing an action plan to achieve a specific health behavior change that they feel is manageable and realistic. BAP is highly structured, using a combination of specific questions and provider-led discussion (called “skills”), all the while staying true to the spirit of MI.
Figure: Brief Action Planning Flow Chart and Checking on the BAP13
BAP can be implemented using different combinations of practice staff in order to make good use of clinic and provider time. For example, a provider may start the conversation during the patient visit, inquiring about the patient’s health goals; if the patient has a health goal in mind, the provider may refer the patient to another practice staff member such as a medical assistant or nurse who has been trained in BAP, to complete the session. The patient can also be referred to Physical Therapy or a weight management clinic. Another approach is for a frontline staff person such as medical assistant to begin the process with the initial question to the patient, allowing the provider to continue the goal-setting part of the conversation with the patient during their visit.12
More information about training opportunities and resources, including videos and example conversations can be found at the Centre for Collaboration, Motivation, & Innovation website.
Counseling models that address specific behaviors within the OA management framework (physical activity and weight management) include Physical Activity as a Vital Sign and the Obesity Canada’s 5 As of Obesity Management.24
Physical Activity as a Vital Sign
Assessing physical activity in patients
EVS: Exercise Vital Sign16
Used in the Kaiser Permanente Southern California health system, providers record patients’ responses in the electronic health record.
Consists of two questions:
1. On average how many days per week do you engage in moderate to strenuous exercise (like a brisk walk)?”
2. On average, how many minutes per day do you engage in exercise at this level?
Scoring: Multiply the responses to get the number minutes per week of exercise and compare this to the PAGs (>150 minutes per week).
For patients with OA, physical activity is particularly important, as it can help improve pain, stiffness, and physical function.14 Patients with OA also often have other chronic diseases like obesity, hypertension, and diabetes. When they engage in physical activity, patients can improve not only their arthritis symptoms but can also make headway on these other chronic conditions. Further, the American College of Rheumatology guidelines for the management of hip and knee OA strongly recommends physical activity as frontline nonpharmacologic management.15 Thus, assessing patients’ current level of physical activity is vital when treating patients with OA, just as measuring blood pressure at each clinic visit is vital to the treatment of hypertension.
There are several initiatives and health systems that encourage providers to assess patients’ current physical activity level and prescribe physical activity for the prevention and management of chronic diseases.3,14 There is not currently a universal approach to this idea of “Physical Activity as a Vital Sign”; however, by using one of several Physical Activity as a Vital Sign measures, providers can quickly assess patients’ current level of physical activity, and in some cases, even assess patients’ readiness and motivation to become more physically active.14 Examples of physical activity assessment tools include:
- Exercise Vital Sign (EVS)16
- Physical Activity Vital Sign (PAVS)17
- Speedy Nutrition and Physical Activity Assessment (SNAP)18
- General Practice Physical Activity Questionnaire (GPPAQ)19
- Stanford Brief Activity Survey (SBAS)20
Regardless of which measure is used, Physical Activity as a Vital Sign can serve as a conversation starter with the patient. After hearing the patient’s answer about current physical activity level, it would be important for the provider to subsequently engage the patient in a conversation about increasing their physical activity level (as appropriate). This could then lead to a referral to another provider (ex. Physical Therapist) or community-based physical activity intervention or perhaps to future counseling sessions to help the patients develop a physical activity plan.
Exercise is Medicine®
Exercise is Medicine® is a global initiative, started in partnership between the American Medical Association and the American College of Sports Medicine, to advance the use of exercise as a prescription for both disease prevention and health promotion. To help facilitate the widespread practice of prescribing physical activity as a regular course of treatment, Exercise is Medicine® has developed a comprehensive guide for physicians and other health care providers. Their Health Care Providers Action Guide incorporates the use of the PAVS questionnaire with motivational interviewing techniques and referrals to community-based physical activity programs.3 This free guide and accompanying patient-facing materials, such as “Being Active when you have Osteoarthritis,” can be found on the Exercise is Medicine® website.
5 As
According to the CDC almost one-quarter of people who are overweight and 30% of people who are obese have arthritis.4 Addressing OA symptoms through weight loss, particularly if a patient’s weight is contributing negatively to other health conditions, could be particularly effective. Weight loss counseling is a key component of successful weight loss among patients. As noted previously, provider counseling is an underused but effective strategy for encouraging adults with arthritis and overweight or obesity to attempt to lose weight.7
The 5 As model was developed for use in smoking and tobacco cessation counseling.21-23 It has since been validated in other areas of behavior change, particularly within the field of weight loss and obesity management.22,23 Obesity Canada has developed an extensive toolkit on the use of 5As of Obesity Management in primary care settings. According to Dr. Arya M. Sharma, scientific director for CON-RCO, (Canadian Obesity Network) “Weight is a sensitive issue, and so conversations about weight must be sensitive and non-judgmental. The 5As tool is based on our understanding that obesity must be managed as a chronic condition, much like diabetes or hypertension, and that treatment goals as well as end results will be different for each patient. But, it all starts with a respectful conversation.”24
“The 5As tool is based on our understanding that obesity must be managed as a chronic condition, much like diabetes or hypertension, and that treatment goals as well as end results will be different for each patient. But, it all starts with a respectful conversation.”24 DR. ARYA M. SHARMA
The primary steps of the 5 As are outlined below. The 5As model can be used in the context of most behavior changes; this example is related to weight loss counseling.
5As of Obesity Management22,24
| ASK Would it be OK if we talk about your weight? Do you have any concerns or questions about your weight? On a scale of 0 to 10, how important is it for you to lose weight? On a scale of 0 to 10, how confident are you that you can lose weight? |
|
| ASSESS Determine patient's stage and level of obesity Review patient's history and records to help determine underlying causes Ask patient questions about diet, sleep, physical activity habits, and emotional health (depression, addiction, trauma, etc) |
|
| ADVISE Discuss with patient the risks of excess weight Discuss with patient the benefits of losing weight Offer options of weight loss strategies (increased physical activity, nutrition counseling, food journal, sleep hygiene, surgery, etc) |
|
| AGREE Help patient set realistic goals based on patient's preferences and abilities Using SMART goals, help patient develop a weight loss plan |
|
| ASSIST Help patient think through potential challenges and personal supports Refer patient to other professionals (mental health, dietician, PT, etc) Refer patient to community-based health programs Make a plan to follow up with patient at a specific timepoint |
Additional Resources for Providers
COACH from USBJI
COACH– Creating Opportunities for Arthritis Control at Home- is a set of training modules designed for providers who see patients with arthritis and want to encourage them to manage arthritis outside the clinic, in their day-to-day lives at home. Drawing on Motivational Interviewing, Brief Action Planning, Stages of Change, and other approaches to behavior change, COACH features techniques that help patients address the risk factors for arthritis as well as many other chronic conditions.
THE ROLE OF WEIGHT BIAS
OAAA Lunch & Learn recorded presentation- “The Role of Weight Bias on Health Outcomes” (Fatima Cody Stanford, MD, MPH, MPA)
UConn’s Rudd Center: informational handouts and videos for providers about weight bias and strategies for talking with patients about weight loss
Harvard’s Implicit Association Tests (IAT) where you can test yourself for different types of bias (ex. race, weight)
MOTIVATIONAL INTERVIEWING
OAAA Lunch & Learn recorded presentation- “The patient will see you now: Managing OA as a chronic disease” (Kim Bennell, PhD)
OAAA Lunch & Learn recorded presentation- “Practical Applications for Motivational Interviewing” (Linda Ehrlich Jones, PhD, RN)
Motivational Interviewing- Enhancing Motivation for Change in Substance Abuse Treatment (Chapter 3- Motivational Interviewing as a Counseling Style)
Kathleen G. Reims, MD, FAAFP, and Denise Ernst, PhD “Using Motivational Interviewing to Promote Healthy Weight,” Fam Pract Manag. 2016 Sep-Oct;23(5):32-38. Available online.
BRIEF ACTION PLANNING
Gutnick D, Reims K, Davis C, Gainforth H, Jay M, Cole S. Brief Action Planning to Facilitate Behavior Change and Support Patient Self-Management. Journal of Clinical Outcomes Management. 2014;21(1):17-29.
YouTube video- Basics of BAP
YouTube video- sample BAP conversation with patient who has Rheumatoid Arthritis
YouTube video- sample BAP conversation with patient who is ambivalent
Centre for Collaboration Motivation & Innovation website
PHYSICAL ACTIVITY AS A VITAL SIGN
Exercise is Medicine®: Health Care Providers Action Guide
OAAA Lunch & Learn recorded presentation- “Exercise is Medicine – The Importance of Connecting Fitness with Healthcare” (Robert Sallis, MD, FAAFP, FACSM)
5 As
Obesity Canada, including a Practitioner Guide
SHARED DECISION MAKING TOOL
The Movement is Life™ Shared Decision support tool is intended to be used with patients with chronic knee pain that is likely knee osteoarthritis. This framework was designed to support a discussion between healthcare providers and patients to help patients see the impact of their treatment choices over time. Patients will receive a projection about their pain and function level if they “do nothing” compared to if they engage in specific treatments such as weight loss, increased physical activity, Physical Therapy and pain medications.
PATIENT RESOURCES
The OAAA offers many resources and tools to help adults find information on understanding OA and managing their symptoms at home and work.
 CLINICAL TAKE-HOME POINTS
CLINICAL TAKE-HOME POINTS
-
-
- Patients who receive counseling from their providers about weight loss and physical activity are more likely to engage in and have positive outcomes from these behavior changes.
- Four tools you can use when counseling patients with OA about lifestyle changes include: Motivational Interviewing, Brief Action Planning, Physical Activity as a Vital sign, and 5 As.
-
REFERENCES
-
- Centers for Disease Control and Prevention. National Center for Health Statistics: Exercise or Physical Activity. Available at https://www.cdc.gov/nchs/fastats/exercise.htm. Published 2017. Accessed February 22, 2019.
- Centers for Disease Control and Prevention. National Center for Health Statistics: Obesity and Overweight. Available at https://www.cdc.gov/nchs/fastats/obesity-overweight.htm. Published 2016. Accessed February 22, 2019.
- Bowen PG, Mankowski RT, Harper SA, Buford TW. Exercise is Medicine as a Vital Sign: Challenges and Opportunities. Transl J Am Coll Sports Med. 2019;4(1):1-7.
- Barbour KE, Helmick CG, Boring M, Brady TJ. Vital Signs: Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation – United States, 2013-2015. MMWR Morb Mortal Wkly Rep. 2017;66(9):246-253.
- Centers for Medicare & Medicaid Services. Report to Congress: the Centers for Medicare & Medicaid Services’ evaluation of community-based wellness and prevention programs under section 4202 (b) of the Affordable Care Act. In. Baltimore, MD: Centers for Medicare & Medicaid Services; 2013.
- Hootman JM, Murphy LB, Omura JD, et al. Health Care Provider Counseling for Physical Activity or Exercise Among Adults with Arthritis – United States, 2002 and 2014. MMWR Morb Mortal Wkly Rep. 2018;66(51-52):1398-1401.
- Guglielmo D, Hootman JM, Murphy LB, et al. Health Care Provider Counseling for Weight Loss Among Adults with Arthritis and Overweight or Obesity – United States, 2002-2014. MMWR Morb Mortal Wkly Rep. 2018;67(17):485-490.
- Rollnick S, Miller WR, Butler C. Motivational interviewing in health care : helping patients change behavior. New York: Guilford Press; 2008.
- Gilbert AL, Lee J, Ehrlich-Jones L, et al. A randomized trial of a motivational interviewing intervention to increase lifestyle physical activity and improve self-reported function in adults with arthritis. Semin Arthritis Rheum. 2018;47(5):732-740.
- Ehrlich-Jones L, Mallinson T, Fischer H, et al. Increasing physical activity in patients with arthritis: a tailored health promotion program. Chronic Illn. 2010;6(4):272-281.
- Reims K, Ernst D. Using Motivational Interviewing to Promote Healthy Weight. Fam Pract Manag. 2016;23(5):32-38.
- Gutnick D, Reims K, Davis C, Gainforth H, Jay M, Cole S. Brief Action Planning to Facilitate Behavior Change and Support Patient Self-Management. Journal of Clinical Outcomes Management. 2014;21(1):17-29.
- Centre for Collaboration Motivation & Innovation. Brief Action Planning Flow Chart. https://centrecmi.ca/wp-content/uploads/2018/11/BAP_flow_Chart_2016-08-08.pdf. Published 2016. Accessed February 19, 2019.
- Golightly YM, Allen KD, Ambrose KR, et al. Physical Activity as a Vital Sign: A Systematic Review. Prev Chronic Dis. 2017;14:E123.
- Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465-474.
- Coleman KJ, Ngor E, Reynolds K, et al. Initial validation of an exercise “vital sign” in electronic medical records. Med Sci Sports Exerc. 2012;44(11):2071-2076.
- Greenwood JL, Joy EA, Stanford JB. The Physical Activity Vital Sign: a primary care tool to guide counseling for obesity. J Phys Act Health. 2010;7(5):571-576.
- Ball TJ, Joy EA, Goh TL, Hannon JC, Gren LH, Shaw JM. Validity of two brief primary care physical activity questionnaires with accelerometry in clinic staff. Prim Health Care Res Dev. 2015;16(1):100-108.
- Heron N, Tully MA, McKinley MC, Cupples ME. Physical activity assessment in practice: a mixed methods study of GPPAQ use in primary care. BMC Fam Pract. 2014;15:11.
- Taylor-Piliae RE, Norton LC, Haskell WL, et al. Validation of a new brief physical activity survey among men and women aged 60-69 years. Am J Epidemiol. 2006;164(6):598-606.
- Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. In: Rockville, MD: US Department of Health and Human Services; May 2008: Available at https://www.ncbi.nlm.nih.gov/books/NBK63952/. Accessed February 22, 2019.
- Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013;59(1):27-31.
- Alexander SC, Cox ME, Boling Turer CL, et al. Do the five A’s work when physicians counsel about weight loss? Fam Med. 2011;43(3):179-184.
- Obesity Canada. 5As of Obesity Management. Available at https://obesitycanada.ca/resources/5as/. Accessed February 22, 2019.