Detection of the signs and symptoms of OA, particularly early detection, can better equip providers and patients in selecting the most appropriate management pathway for both the OA symptoms and other comorbid conditions.
DOWNLOAD PDF
Osteoarthritis (OA) is a complex disease affecting bone, cartilage, meniscus, synovial tissues, tendon/ligament and muscle in and around the whole joint, which has been likened to “joint failure.”1,2 Many of the risk factors are well-established, including aging, joint injury, genetics, gender, anatomic factors, and presence of comorbid chronic conditions.3,4
OA can be diagnosed and characterized using a combination of three data sources:
- Patient symptoms and history
- Physical examination
- Imaging evaluation
Patient Symptoms and History
Patients may report obvious symptoms of OA such as pain and stiffness in certain joints, but more nuanced symptoms indicative of the condition may arise during a comprehensive history and physical (functional changes, sleep disturbances, history of joint injury, comorbidities).
PAIN AND STIFFNESS
Common Symptoms of OA
- Sore or stiff joints – particularly the hips, knees, and lower back – after inactivity or overuse.
- Limited range of motion or stiffness that goes away after movement
- Clicking or cracking sound when a joint bends
- Mild swelling around a joint
- Pain that is worse after activity or toward the end of the day
The joint sites most often affected by OA include the hands, hips, knees, feet, and spine. Symptoms vary based on the affected joint(s) and the severity of the condition. Pain is a frequent complaint.5,6 Typically, patients with mild OA experience localized, insidious pain that is relieved by rest, but aggravated by activity. Although OA is not necessarily progressive, in more moderate to severe forms, the intensity of the pain can vary, especially at night when activity has been high throughout the day.7 OA pain may be neuropathic in nature indicated by a sensation of burning or “pins and needles.”8 OA may be either unilateral or bilateral, but often affects multiple joints.
Joint stiffness (although generally less than 30 minutes’ duration) and limited range of motion are also frequent complaints. Affected joints may get swollen, especially after extended activity. These symptoms tend to build over time rather than show up suddenly.
OA can affect multiple joints of the body in different ways:
- Hips- Pain is felt in the groin area or buttocks and sometimes on the inside of the knee or thigh; stiffness after sitting
- Knees- A grating or scraping sensation can occur when moving the knee; stiffness after sitting.
- Hands- Bony enlargement (nodes) can cause fingers to become swollen/enlarged and tender. There may be pain at the base of the thumb.
- Feet- Pain and tenderness are felt in the large joint at the base of the big toe and in the mid-foot. There may be swelling in ankles or toes.
ACTIVITIES OF DAILY LIVING AND FUNCTIONAL CHANGES
 OA pain, swelling or stiffness may make it difficult to perform ordinary tasks at work or at home.9 Simple acts like tucking in bed sheets, opening a box of food, grasping a computer mouse or driving a car can become nearly impossible. When the lower body joints are affected, activities such as walking, climbing stairs and lifting objects may become difficult. When finger and hand joints are affected, OA can make it difficult to grasp and hold objects, such as a pencil, or to do delicate tasks, such as needlework or fastening clothes.
OA pain, swelling or stiffness may make it difficult to perform ordinary tasks at work or at home.9 Simple acts like tucking in bed sheets, opening a box of food, grasping a computer mouse or driving a car can become nearly impossible. When the lower body joints are affected, activities such as walking, climbing stairs and lifting objects may become difficult. When finger and hand joints are affected, OA can make it difficult to grasp and hold objects, such as a pencil, or to do delicate tasks, such as needlework or fastening clothes.
OA can have social consequences for a person, interfering with activities of daily living, visiting with friends and relatives, and participating in the larger community.10
Hawker et al7 describe 3 stages of OA based on patient-reported pain and functional limitations:
- Early OA: patients experience infrequent and predictable but sharp pain brought on by specific movements or activities like high impact sports; usually they still have well-preserved joint function and quality of life (QOL).
- Mid-OA: patients continue to experience predictable, but more constant, pain and also start having unpredictable symptoms such as locking. These symptoms begin to impair functionality, participation in activities, and QOL.
- Advanced OA: patients have persistent dull and aching pain with intermittent episodes of unpredictable sharp pain. They experience fatigue along with impaired functionality and are significantly restricted in activities and QOL. 7
Patients may also report sleep disturbances characteristic of insomnia (inadequate sleep, sometimes including difficulty initiating or maintaining sleep) and feeling unrefreshed (or nonrestorative; lack of satisfaction with the sleep experience).11 The prevalence of sleep disturbance among people with knee OA is estimated at more than 70%.11
HISTORY OF JOINT INJURY
Patients with a history of joint injury are at increased risk of developing arthritis. Post-traumatic arthritis makes up approximately 12% of all OA cases and can result from injuries sustained in automobile or military accidents, falls, or sports.12 Someone with a history of anterior cruciate ligament (ACL) or meniscus tear is 2.5 times more likely to develop knee OA and four times more likely to undergo an eventual total knee arthroplasty.13-15 Within the first decade after an ACL injury about 1 in 3 patients have radiographic OA, regardless of initial treatment strategy.16,17
COMORBIDITIES
The connection between OA and many other chronic conditions is strong. The presence of other comorbid conditions can serve as an indicator that a patient may have OA or is at risk of developing OA, or that comorbid conditions may complicate OA management. See the Comorbidities and Co-Occurring Symptoms module for more information about OA & other comorbid conditions.
Physical Examination
JOINT APPEARANCE
On physical exam, the affected joint(s) may appear normal; however, tenderness, pain or mild swelling could be present. Joints with OA are not usually appreciably warm, red, or largely swollen; however, swelling and tenderness may occur. Crepitus, a crackling or grinding within a joint, may be palpable. Muscle wasting (e.g., of quadriceps or thenar muscles) or joint deformity (due to bony enlargement, ankylosis, or malalignment) may also be present. Osteophytes can be palpated as bony projections, and may result in deformities, especially in the distal interphalangeal and proximal interphalangeal joints in the hands. Such deformities may eventually restrict joint range of motion.18
Heberden’s & Bouchard’s Nodes
Patients with hand OA may present with Heberden’s and/or Bouchard’s nodes, which represent bony enlargement of the distal or proximal interaphalangeal joints, respectively. Such nodes are more common in women and patients with multiple joint OA.

Copyright 2019. American College of Rheumatology. Used with permission.
DIFFERENTIAL DIAGNOSIS
When a patient presents with complaints of “joint pain,” certain key elements should be evaluated to best direct care. Table 1 illustrates distinguishing characteristics between OA and other common forms of arthritis such as rheumatoid arthritis (RA) and gout or crystalline arthritis. If a patient presents with symptoms or has laboratory (e.g., serum) markers characteristic of inflammatory arthritis, prompt referral to their primary care provider is recommended for further evaluation, as it could indicate the presence of RA or acute gout.
Table 1: Comparison of Osteoarthritis, Rheumatoid Arthritis, and Acute Gout19
| Characteristic | Osteoarthritis | Rheumatoid Arthritis | Acute Gout |
|---|---|---|---|
| Visible signs of inflammation | None or very mild | Often present | Yes |
| Onset of pain | Gradual (months to years) | Gradual (weeks to months) | Often sudden (frequently overnight) |
| Inactivity stiffness | < 30 minutes | > 30 minutes | Unpredictable |
| Systemic Symptoms | No | Yes | Not routinely |
| Initial number of affected joints | Often 1-2 | 2+ (bilateral, symmetrical) | 1 (often the great toe) |
| Common joint involvement | Distal hands, basal thumb, knees, hip, spine | Feet, ankles, proximal hands, wrists, ankles, feet | Hands, wrists, elbows, knee, ankle, great toe |
ASSOCIATED EXAM FINDINGS
Functional assessments
There is no single measure to assess a patient’s physical function in the setting of research or clinical care for OA. However, using a combination of performance measures and patient-reported outcome measures (PROMs) may give the healthcare provider insight into disease progression, severity, and optimal treatment approaches. Performance measures assess what patients can do as opposed to what they think they can do.40 PROMs are questionnaires that patients complete to describe how arthritis impacts their lives.41 It has been suggested that PROMs reveal patients’ perceived experiences with the disease and its impact on specific activities rather than their actual ability to perform the activities.42 Patient self-reports may be influenced by pain, stiffness, and feeling of exertion (not just ability or difficulty in performing the task).42 The use of PROMs in clinical care lends itself to shared decision-making. In addition, the process of engaging patients in self-reporting may result in improved self-management, quality of life, satisfaction of care, and communication.43 The following supplemental resources on functional assessments in OA care are available in this toolkit: Overview of Functional Assessments for Knee & Hip OA, Practical Use of Functional Assessments in OA Care, In-depth description of available assessments organized by joint.
Gait Assessment & Malalignment
When a patient’s gait is observed in the clinic, an uneven or unstable gait may be noted. Additionally, malalignment (i.e., varus [bowlegged] or valgus [knock-kneed]) can result in increased risk of development or progression of knee OA. The worse the malalignment, the greater decline in physical function likely to be experienced by patients.20 Issues of alignment and gait may be better assessed by PT referral. See the Clinical Management of OA module for more information about referrals.
Quadriceps strength
Reduced quadriceps strength has been connected to increased functional disability and pain in people with knee OA21,22 and is a risk factor for both OA and falls in the older population.23 Muscle-strengthening exercises, whether with a physical therapist or through a community-based intervention program, can help reduce pain and functional limitations.
Imaging Evaluation
Medical history and clinical exam may indicate further exploration via various imaging modalities to confirm or refine an OA diagnosis, although this is often not necessary. Imaging is generally not needed to guide treatment decisions. Patients with OA may experience debilitating symptoms but have little radiographic evidence supporting OA or they may have significant radiographic evidence but few symptoms.24 Radiographs can be considered to confirm the diagnosis in the case of uncertainty or other potential etiologies (e.g., evaluation for osteonecrosis or fracture); more advanced imaging is rarely indicated clinically.
X-RAYS
Plain radiograph, or x-ray, is the most common, cost-effective, and accessible form of imaging for OA, but it is not without limitations. X-rays are useful for viewing two-dimensional structural changes, which can be helpful in diagnosing OA because the affected joint will have a characteristic appearance:
-
-
- Osteophytes (bone spurs) often develop at joint margins and are one of the key features of OA in any affected joint
- Joint space narrowing can be seen at any affected joint and often reflects cartilage thinning, damage, or total loss. At the knee, the joint space can appear narrowed due to meniscal damage and extrusion. Joint space narrowing can be affected by the radiographic view and patient positioning.
- Subchondral cysts and sclerosis indicate damage to the underlying subchondral bone, often adjacent to an area with cartilage damage.
- Joint malalignment or deformity can be risk factors (e.g., varus malalignment) or consequences of the OA process from damage to the joints over time.
-
X-ray images do not show soft tissues, nor can they discern early signs of OA. Structural changes that are detectable on plain radiograph are generally indicative of a later, more advanced disease state.2
Sample knee radiographs
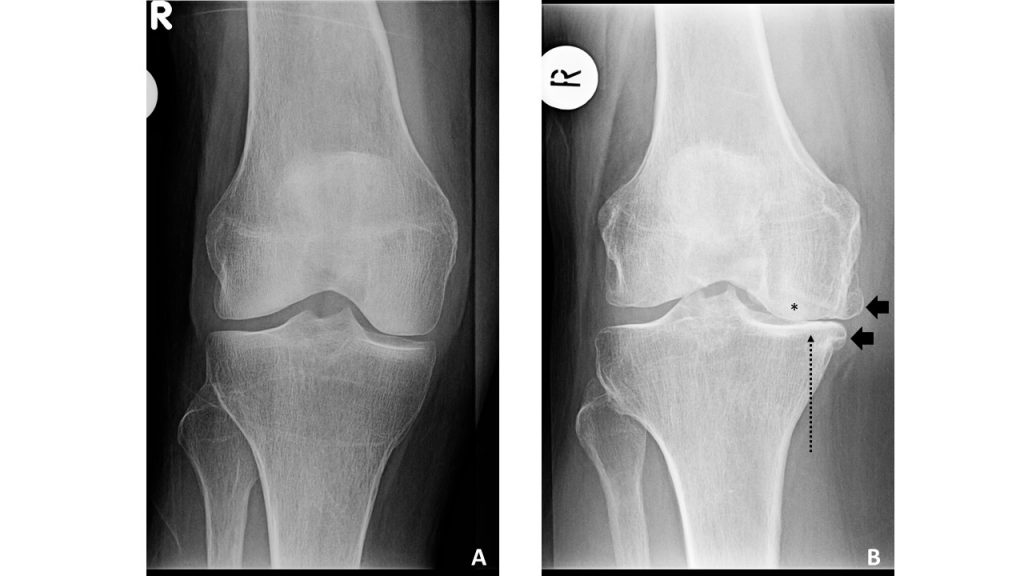
B. Right knee with KLG=4, with sclerosis (*), medial joint space narrowing (long dashed arrow), osteophytes (black arrows)
Images from the Johnston County Osteoarthritis Project, courtesy of Amanda E. Nelson MD MSCR
ADVANCED IMAGING MODALITIES
While MRI (magnetic resonance imaging), CT (computed tomography) and US (ultrasound) are sensitive modalities for detecting a variety of changes in the OA joint, they are not indicated for clinical use. These modalities are, however, very useful in research given their greater resolution, sensitivity, and ability to detect changes early in the disease process. Such information may prove useful for identifying subgroups (or phenotypes) of OA that may be more likely to respond to given treatments as novel interventions are developed. Additionally, US is useful as a point-of-care tool for intervention guidance25 (e.g., intra-articular injections into deep or difficult joints).
Early Detection and Treatment
Symptomatic OA and radiographic OA do not always overlap: patients with radiographic OA may not suffer from OA symptoms, and patients may experience OA symptoms before the disease is evident by examination or on imaging studies.
Patient-reported symptoms of pain and associated disability are the more important indicators for providers to use in diagnosing OA and helping patients begin to manage their symptoms and functional limitations.26
However, OA can develop over many years, and even before a patient expresses signs and symptoms of OA, it is important for providers to be aware of potential risk factors and intervene with patients on a preventative level.27,28 Patients at particular risk of developing OA are those who have suffered an ACL injury or intra-articular fracture, those with hip dysplasia27 or cam morphology29 as well as those who are overweight3,30-33 or who have participated in occupational or athletic activities that involve repetitive or excessive joint loading.34-37 It is important to engage these patients in prevention and self-management strategies as early as possible to manage their symptoms and prevent or delay the progression of OA.
Connect patients to self-management activities and programs

Participation in community-based programs that support self-management education and increasing physical activity have been shown to help with symptom management and preventing or delaying the progression of OA. The Clinical Management of OA and Community and Patient Resources modules provide information about programs that are recommended by the CDC, as well as guidance on how to locate these programs in your community.
Pain management to improve quality of life and management of other chronic diseases
A patient’s ability or desire to participate in exercise therapy (e.g., cardiac rehabilitation, regular physical activity) as a treatment option for cardiovascular disease, diabetes, or obesity may be limited as a result of OA-related pain and functional limitations. It is important for providers to assess patients presenting with other chronic conditions for the presence of joint pain to identify and address this barrier to exercise. Providers can reassure patients that exercising with OA is safe and provide resources to patients about specialized interventions, such as aquatic therapy38 or Walk With Ease39. The Resources for People with Arthritis handout includes more information about these programs and additional resources. Providers can also recommend appropriate pain control measures like APAPs or NSAIDs with specific instructions about dosing around exercise sessions.
ADDITIONAL READING
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745-1759.
CLINICAL TAKE-HOME POINTS
![]()
-
-
- OA is a clinical diagnosis, characterized by pain, aching, and stiffness most often affecting the knees, hips, back, hands, and feet.
- When imaging is needed, radiographs are usually sufficient to rule out other etiologies and confirm the diagnosis.
- Early detection of OA is beneficial for engaging patients in prevention and self-management strategies as early as possible to manage their symptoms and prevent or delay the progression of OA.
-
REFERENCES
-
- Nuki G. Osteoarthritis: a problem of joint failure. Z Rheumatol. 1999;58(3):142-147.
- Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64(6):1697-1707.
- Loeser R. Pathogenesis of osteoarthritis. In: Post T, ed. UpToDate. Waltham, Mass: UpToDate; 2018: https://www.uptodate.com/contents/pathogenesis-of-osteoarthritis. Accessed June 20, 2022.
- Centers for Disease Control and Prevention. Osteoarthritis. Available at http://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Published 2019. Updated February 21, 2019. Accessed.
- Arthritis Foundation. Diagnosing osteoarthritis. Available at https://www.arthritis.org/about-arthritis/types/osteoarthritis/diagnosing.php. Accessed June 12, 2018.
- Johns Hopkins Arthritis Center. Osteoarthritis: Signs and symptoms. Available at https://www.hopkinsarthritis.org/arthritis-info/osteoarthritis/signs-and-symptoms/. Accessed Accessed June 4, 2018.
- Hawker GA, Stewart L, French MR, et al. Understanding the pain experience in hip and knee osteoarthritis–an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16(4):415-422.
- Hochman JR, Gagliese L, Davis AM, Hawker GA. Neuropathic pain symptoms in a community knee OA cohort. Osteoarthritis Cartilage. 2011;19(6):647-654.
- McDonough CM, Jette AM. The contribution of osteoarthritis to functional limitations and disability. Clin Geriatr Med. 2010;26(3):387-399.
- Theis KA, Murphy L, Hootman JM, Wilkie R. Social participation restriction among US adults with arthritis: a population-based study using the International Classification of Functioning, Disability and Health. Arthritis Care Res (Hoboken). 2013;65(7):1059-1069.
- Allen KD, Renner JB, Devellis B, Helmick CG, Jordan JM. Osteoarthritis and sleep: the Johnston County Osteoarthritis Project. J Rheumatol. 2008;35(6):1102-1107.
- Punzi L, Galozzi P, Luisetto R, et al. Post-traumatic arthritis: overview on pathogenic mechanisms and role of inflammation. RMD Open. 2016;2(2):e000279.
- Buys LM, Wiedenfeld SA. Osteoarthritis. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, M P, eds. Pharmacotherapy: A Pathophysiologic Approach, 10e. New York, NY: McGraw-Hill.
- Vina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol. 2018;30(2):160-167.
- Hunter DJ, Zhang YQ, Niu JB, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54(3):795-801.
- Luc B, Gribble PA, Pietrosimone BG. Osteoarthritis prevalence following anterior cruciate ligament reconstruction: a systematic review and numbers-needed-to-treat analysis. J Athl Train. 2014;49(6):806-819.
- Harris KP, Driban JB, Sitler MR, Cattano NM, Balasubramanian E, Hootman JM. Tibiofemoral Osteoarthritis After Surgical or Nonsurgical Treatment of Anterior Cruciate Ligament Rupture: A Systematic Review. J Athl Train. 2017;52(6):507-517.
- Hunter DJ, Felson DT. Osteoarthritis. BMJ. 2006;332(7542):639-642.
- Venables P, BChir M. Diagnosis and differential diagnosis of rheumatoid arthritis. In. UpToDate. Waltham, Mass: UpToDate; 2018.
- Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188-195.
- O’Reilly SC, Jones A, Muir KR, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis. 1998;57(10):588-594.
- Bacon KL, Segal NA, Oiestad BE, et al. Thresholds in the relationship of quadriceps strength with functional limitations in women with knee osteoarthritis. Arthritis Care Res (Hoboken). 2018.
- Ahmadiahangar A, Javadian Y, Babaei M, Heidari B, Hosseini S, Aminzadeh M. The role of quadriceps muscle strength in the development of falls in the elderly people, a cross-sectional study. Chiropr Man Therap. 2018;26:31.
- Block JA. Chapter 181: Clinical Features of Osteoarthritis. In: Hochberg MC, Gravellese EM, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH, eds. Rheumatology, 7th edition. Philadelphia, PA: Elsevier; 2019.
- Finnoff JT, Hall MM, Adams E, et al. American Medical Society for Sports Medicine (AMSSM) position statement: interventional musculoskeletal ultrasound in sports medicine. Br J Sports Med. 2015;49(3):145-150.
- Nelson AE, Elstad E, DeVellis RF, et al. Composite measures of multi-joint symptoms, but not of radiographic osteoarthritis, are associated with functional outcomes: the Johnston County Osteoarthritis Project. Disabil Rehabil. 2014;36(4):300-306.
- Chu CR, Millis MB, Olson SA. Osteoarthritis: From Palliation to Prevention: AOA Critical Issues. J Bone Joint Surg Am. 2014;96(15):e130.
- Chu CR, Williams AA, Coyle CH, Bowers ME. Early diagnosis to enable early treatment of pre-osteoarthritis. Arthritis Res Ther. 2012;14(3):212.
- Agricola R, Waarsing JH, Arden NK, et al. Cam impingement of the hip: a risk factor for hip osteoarthritis. Nat Rev Rheumatol. 2013;9(10):630-634.
- Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil. 2006;85(11 Suppl):S2-11; quiz S12-14.
- Johns Hopkins Arthritis Center. Role of body weight in osteoarthritis. Available at https://www.hopkinsarthritis.org/patient-corner/disease-management/role-of-body-weight-in-osteoarthritis/. Accessed June 4, 2018.
- Messier SP, Gutekunst DJ, Davis C, DeVita P. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005;52(7):2026-2032.
- Messier SP, Mihalko SL, Legault C, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263-1273.
- Yucesoy B, Charles LE, Baker B, Burchfiel CM. Occupational and genetic risk factors for osteoarthritis: a review. Work. 2015;50(2):261-273.
- Cameron KL, Driban JB, Svoboda SJ. Osteoarthritis and the Tactical Athlete: A Systematic Review. J Athl Train. 2016;51(11):952-961.
- Amoako AO, Pujalte GG. Osteoarthritis in young, active, and athletic individuals. Clin Med Insights Arthritis Musculoskelet Disord. 2014;7:27-32.
- Driban JB, Hootman JM, Sitler MR, Harris KP, Cattano NM. Is Participation in Certain Sports Associated With Knee Osteoarthritis? A Systematic Review. J Athl Train. 2017;52(6):497-506.
- Rahmann AE. Exercise for people with hip or knee osteoarthritis: a comparison of land-based and aquatic interventions. Open Access J Sports Med. 2010;1:123-135.
- Arthritis Foundation. Walk With Ease. Available at https://www.arthritis.org/living-with-arthritis/tools-resources/walk-with-ease/. Accessed June 25, 2019.
- Dobson F, et al. Osteoarthritis Cartilage. 2013;21(8):1042-1052.
- Lundgren-Nilsson et al. RMD Open. 2018;4(2):e000715.
- Stratford PW, et al. Phys Ther. 2006;86(11):1489-1496.
- American Academy of Orthopaedic Surgeons (AAOS). 2017 Osteoarthritis: Function & Pain Assessment Measure Methodology Report. In: Rosemont, IL. 2017.