Osteoarthritis is common and increasing in prevalence, resulting in enormous personal and societal costs.
DOWNLOAD PDF OA Disparities RecordingAdditional Resources: Learn more about the burden of OA to employers and working adults
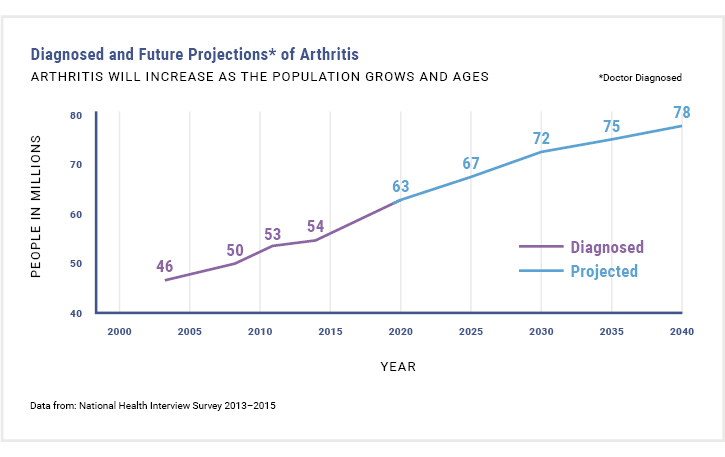
Arthritis is a serious health crisis. CDC estimates that 1 in 5 (or 53.2 million) US adults have some form of arthritis.1 While there are estimated to be more than 100 types of arthritis, osteoarthritis (OA) is the most common form of arthritis, affecting 32.5 million US adults.2 The high prevalence of arthritis manifests in enormous societal and personal costs.
Figure 1: Future Projections of Arthritis3
PREVALENCE BY AGE, GENDER, AND ETHNICITY
Age
- 43% of people with OA are 65 or older and 88% of people with OA are 45 or older.2
- Annual incidence of knee OA is highest between 55 and 64 years old.6
- More than half of individuals with symptomatic knee OA are younger than 65.6
Gender
- 62% of individuals with OA are women.2
- Among people younger than 45, OA is more common among men; above age 45, OA is more common in women.6
Ethnicity
- 78% of individuals with OA are non-Hispanic whites.2
- However, within their own race/ethnic groups, non-Hispanic black and Hispanic populations have higher rates of OA than non-Hispanic whites.2
- Documented racial disparities exist in musculoskeletal health, with arthritis having a greater impact on People of Color than Whites.12,13,18
- See Patient Burden/Activity & Work Limitations below for more details on racial disparities in OA.
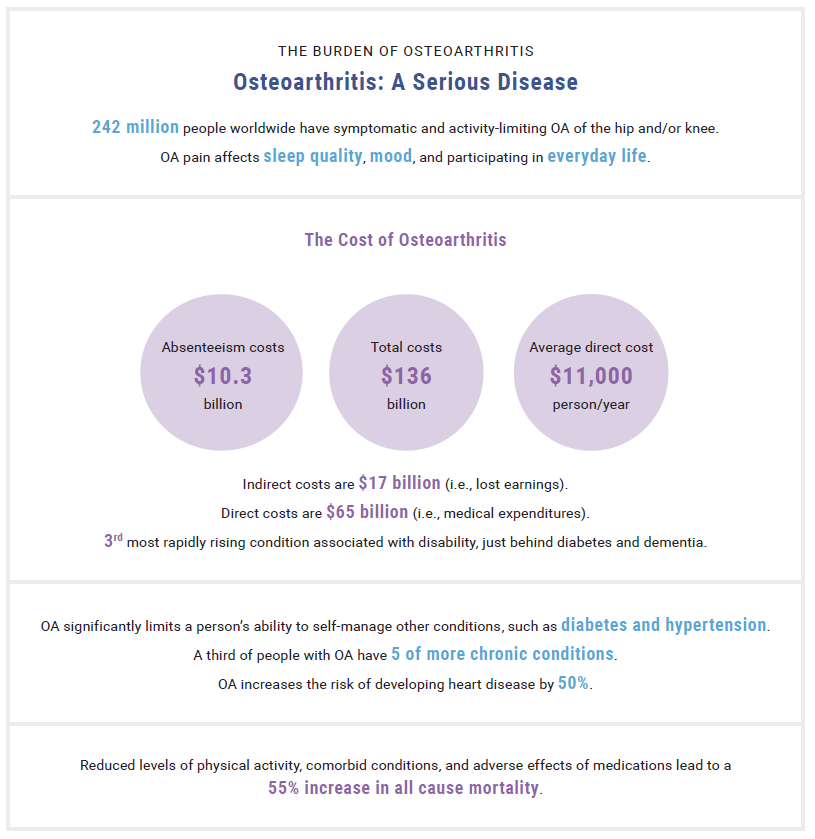
THE BURDEN OF OSTEOARTHRITIS2,4
Download a similar version of this infographic as a PDF or PNG.
PATIENT BURDEN
Pain
- People with OA experience greater pain, fatigue, levels of disability, and
 activity limitations than people of their comparable age.4
activity limitations than people of their comparable age.4 - While arthritis pain is extremely individualized, severe joint pain is not uncommon. Recent estimates suggest that one-fourth of adults with arthritis experience severe joint pain, characterized by a score of 7 or greater on the 0-10 pain scale.5
- Severe joint pain occurs more often in middle-aged adults (45-64), women, non-Hispanic blacks, Hispanics, those with a disability, and in people with the following concurrent health conditions: fair/poor health, obesity, diabetes, heart disease, and serious psychological distress.5
- 99% of all hip and knee replacements are done to address pain and functional limitations.18
- Over 50% of people with knee OA will have a total knee replacement done during their lifetime.6
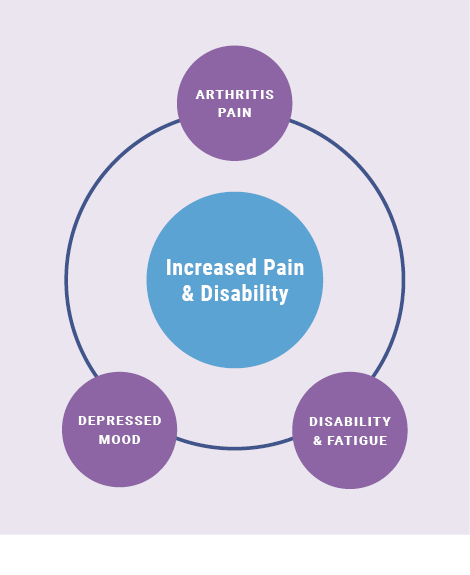
Pain- both chronic and episodic- can result in depression and other mood disturbances, functional disabilities, and work limitations.
Depression and Social Isolation
- One-third of people with arthritis over the age of 45 suffer from depression or anxiety.18
- People with OA are likely at greater risk for depression because of increased disability and fatigue associated with their pain.7
- People with doctor-diagnosed arthritis report more days in the last month of poor mental health (5.4 days vs 2.8 days for people without arthritis).2
- Social isolation and loneliness are often evident among people with osteoarthritis and other chronic musculoskeletal diseases. There appears to be a bi-directional relationship with pain impacting social isolation and loneliness, and vice versa.8
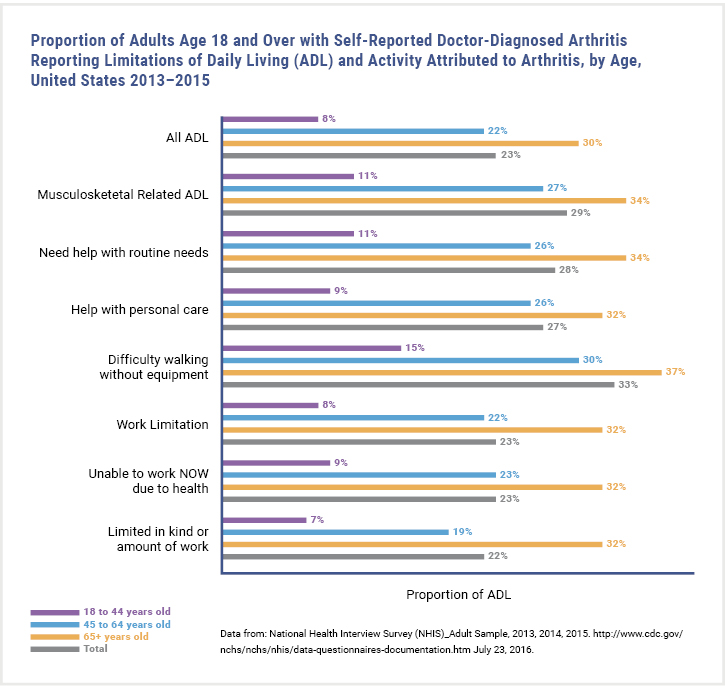
Activity Limitations
- Almost 44% of people with arthritis have “arthritis-attributable activity limitations,” defined as self-reported limitations in “usual activities” because of arthritis symptoms1
- By 2040, 11.4% of all adults will experience arthritis-attributable activity limitations (AAALs).9
- Blacks with knee OA have greater prevalence, severity, progression, and worse pain and function compared with Whites.14
- Non-Hispanic American Indian or Alaska Natives report the highest prevalence of arthritis-attributable activity limitations of any population in the U.S.15
Work Limitations18
- 30% of adults with arthritis find stooping, bending, or kneeling very difficult.
- 20% cannot or find it very difficult to walk 3 blocks or push/pull large objects.
- People with OA (working age) experience lower employment rates than those without OA. Research suggests that arthritis-related activity limitations might contribute to their lack of employment.
- Latinos are more likely to report greater pain, functional limitations, and work limitations than non-Latino Whites.12,15,16
Figure 2: Arthritis-Attributed Limitations2
ECONOMIC BURDEN
The overall economic burden associated with OA in the US is estimated at $136.8 billion annually.2 This stunning figure has more than doubled over the last decade. For perspective, the annual economic cost of arthritis surpasses that of tobacco-related health effects, cancer, and diabetes. Direct medical costs reach $65 billion annually, with annual all-cause per person direct costs reaching $11,502.2
- Because of OA, an estimated 1 million knee and hip replacements are completed each year.18
- Knee OA contributes to more than $27 billion in health care costs each year.6
- In 2013, OA was the 2nd most costly health condition treated in hospitals in the US, accounting for 4.3% of all hospitalization costs.10
- In 2013, total lost wages due to any form of arthritis were $164 billion, or $4,040 less per adult with arthritis compared to those without.10
- Increased absenteeism among workers with OA is fairly well documented, with workers with OA missing an average of 2 more days per year than workers without OA. Presenteeism, or loss of productivity while on the job, is less easy to calculate but is no less costly for workers or businesses.11
 CLINICAL TAKE-HOME POINTS
CLINICAL TAKE-HOME POINTS
-
-
- Arthritis is a serious disease resulting in enormous societal and personal costs.
- Pain from OA can result in depression and other mood disturbances, functional disabilities, and work limitations.
- The overall economic burden of OA in the US is estimated at almost $140 billion annually.
-
REFERENCES
-
- Fallon EA, Boring MA, Foster AL, et al. Prevalence of Diagnosed Arthritis — United States, 2019–2021. MMWR Morb Mortal Wkly Rep 2023;72:1101–1107.
- United States Bone and Joint Initiative. The Burden of Musculoskeletal Diseases in the United States (BMUS). In: In. Fourth ed. Rosemont, IL. 2018: Available at https://www.boneandjointburden.org/fourth-edition. Accessed June 12, 2019.
- Centers for Disease Control and Prevention. 2003 National Health Interview Survey; 2030 Census projected population. Available at https://www.cdc.gov/arthritis/data_statistics/national-statistics.html. Accessed January 19, 2019.
- Osteoarthritis Research Society International. Osteoarthritis: A Serious Disease, submitted to the U.S. Food and Drug Administration. 2016. https://www.oarsi.org/sites/default/files/docs/2016/oarsi_white_paper_oa_serious_disease_121416_1.pdf. Accessed March 27, 2019.
- Barbour KE, Boring M, Helmick CG, Murphy LB, Qin J. Prevalence of Severe Joint Pain Among Adults with Doctor-Diagnosed Arthritis – United States, 2002-2014. MMWR Morb Mortal Wkly Rep. 2016;65(39):1052-1056.
- Arthritis Foundation. Arthritis by the Numbers. In: Atlanta, GA: Arthritis Foundation; 2019: https://www.arthritis.org/getmedia/e1256607-fa87-4593-aa8a-8db4f291072a/2019-abtn-final-march-2019.pdf. Accessed May 13, 2022.
- Hawker GA, Gignac MA, Badley E, et al. A longitudinal study to explain the pain-depression link in older adults with osteoarthritis. Arthritis Care Res (Hoboken). 2011;63(10):1382-1390.
- Smith TO, Dainty JR, MacGregor A. Trajectory of social isolation following hip fracture: an analysis of the English Longitudinal Study of Ageing (ELSA) cohort. Age Ageing. 2018;47(1):107-112.
- Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA. Updated Projected Prevalence of Self-Reported Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation Among US Adults, 2015-2040. Arthritis Rheumatol. 2016;68(7):1582-1587.
- Centers for Disease Control and Prevention. Arthritis Cost Statistics Available at https://www.cdc.gov/arthritis/data_statistics/cost.htm. Published 2018. Accessed January 19, 2019.
- Menon J. Osteoarthritis related absenteeism and activity limitations. Osteoarthritis and Cartilage. 2015;23:A343.
- Bolen J, Schieb L, Hootman JM, et al. Differences in the prevalence and severity of arthritis among racial/ethnic groups in the United States, National Health Interview Survey, 2002, 2003, and 2006. Prev Chronic Dis. 2010;7(3):A64.
- Huff T, Scott M. Musculoskeletal Health Disparities in America. MOJ Orthopedics & Rheumatology. 2017;7(6):00290.
- Callahan LF, Cleveland RJ, Allen KD, Golightly Y. Racial/Ethnic, Socioeconomic, and Geographic Disparities in the Epidemiology of Knee and Hip Osteoarthritis. Rheumatic Disease Clinics of North America. 2021;47(1):1-20.
- Theis KA, Murphy LB, Guglielmo D, et al. Prevalence of Arthritis and Arthritis-Attributable Activity Limitation – United States, 2016-2018. MMWR Morb Mortal Wkly Rep. 2021;70(40):1401-1407.
- Guglielmo D, Murphy L, Boring M, et al. State-Specific Severe Joint Pain and Physical Inactivity Among Adults with Arthritis — United States, 2017. MMWR Morb Mortal Wkly Rep 2019. 2017;68:381-387. DOI: http://dx.doi.org/10.15585/mmwr.mm6817a2.
- Ferucci ED, Schumacher MC, Lanier AP, et al. Arthritis prevalence and associations in American Indian and Alaska Native people. Arthritis Rheum. 2008;59(8):1128-1136.
- Barbour KE, Helmick CG, Boring M, Brady TJ. Vital Signs: Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation—United States, 2013–2015. MMWR Morb Mortal Wkly Rep. 2017;66(9):246-253.