WWE Toolkit Module 2
The information in this section is information regarding the prevalence and burden of arthritis, in general, and information specific to osteoarthritis (OA). PLEASE NOTE: Information and statistics presented here were originally published in OACareTools: A toolkit on osteoarthritis prevention and management in primary care.
Knowing these statistics and being able to clearly communicate them to leadership and collaborators helps to make the case for conducting health promotion programs like Walk With Ease. Areas addressed include:
- Prevalence by age, gender and ethnicity
- Infographic: The burden of osteoarthritis patient burden in terms of pain, social isolation/depression, activity limitations, work limitations
- Economic costs
- Osteoarthritis is associated with increased comorbidity and mortality
Additional materials for making the case are available in the resource library under the tab: Making the Case. Materials are updated as available and currently include
- State Fact Sheets on the Burden of OA
- Arthritis Foundation’s Arthritis Facts
- CDC’s Arthritis Program Data & Statistics
- CDC Vital Signs: Arthritis in America(Spanish)
- CDC Vital Sign Fact Sheet
- CDC Arthritis Press Room
- CDC 500 Cities Project
- DHHS Physical Activity Guidelines for Americans
- NPAPA National Physical Activity Plan
- Economic Cost of Arthritis PowerPoint
- Engaging Veterans in Evidence-Based Programs
Prevalence and Burden of Arthritis
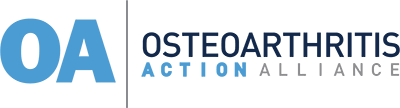
Arthritis is a serious health crisis. CDC estimates that 1 in 4 (or 54.4 million) US adults have some form of arthritis, a figure that is projected to reach 78 million by the year 2040.1 While there are estimated to be more than 100 types of arthritis, osteoarthritis (OA) is the most common form of arthritis, affecting 32.5 million US adults.2 The high prevalence of arthritis manifests in enormous societal and personal costs.
Figure 13
Prevalence by Age, Gender, and Ethnicity1
Age
- 43% of people with OA are 65 or older and 88% of people with OA are 45 or older.2
- Annual incidence of knee OA is highest between 55 and 64 years old.4
- More than half of individuals with symptomatic knee OA are younger than 65.4
Gender
- 62% of individuals with OA are women.2
- Among people younger than 45, OA is more common among men; above age 45, OA is more common in women.4
Ethnicity
- 78% of individuals with OA are non-Hispanic whites.2
- However, within their own race/ethnic groups, non-Hispanic black and Hispanic populations have higher rates of OA than non-Hispanic whites.2
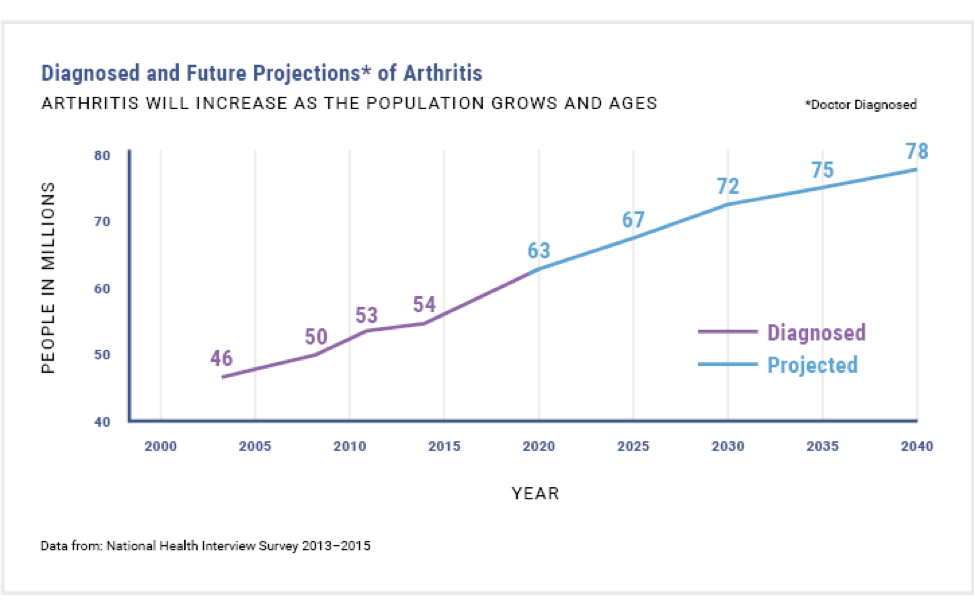
The Burden of Osteoarthritis2,5
Patient Burden
Pain
- People with OA experience greater pain, fatigue, levels of disability, and activity limitations than people of their
 comparable age.5
comparable age.5 - While arthritis pain is extremely individualized, severe joint pain is not uncommon. Recent estimates suggest that one-fourth of adults with arthritis experience severe joint pain, characterized by a score of 7 or greater on the 0-10 pain scale.6
- Severe joint pain occurs more often in middle-aged adults (45-64), women, non-Hispanic blacks, Hispanics, those with a disability, and in people with the following concurrent health conditions: fair/poor health, obesity, diabetes, heart disease, and serious psychological distress.6
- 99% of all hip and knee replacements are done to address pain and functional limitations1
- Over 50% of people with knee OA will have a total knee replacement done during their lifetime.4
Depression and Social Isolation
- One-third of people with arthritis over the age of 45 suffer from depression or anxiety.1
- People with OA are likely at greater risk for depression because of increased disability and fatigue associated with their pain.7
- People with doctor-diagnosed arthritis report more days in the last month of poor mental health (5.4 days vs 2.8 days for people without arthritis).2
- Social isolation and loneliness are often evident among people with OA and other chronic musculoskeletal diseases. There appears to be a bi-directional relationship with pain impacting social isolation and loneliness, and vice versa.8
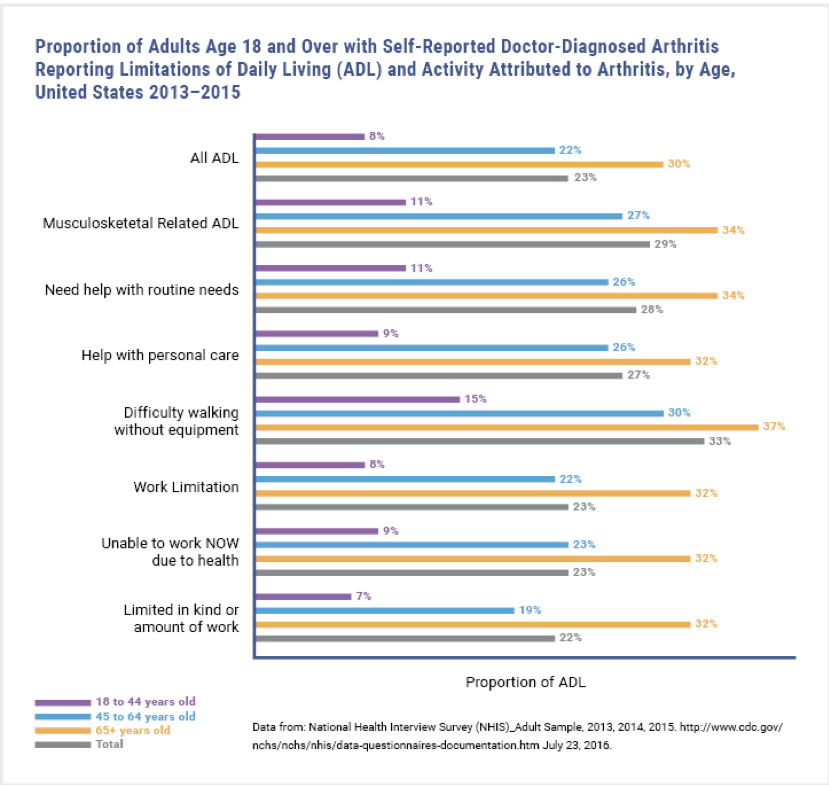
Activity limitations
- Almost 44% of people with arthritis have “arthritis-attributable activity limitations,” defined as self-reported limitations in “usual activities” because of arthritis symptoms1
- By 2040, 11.4% of all adults will experience arthritis-attributable activity limitations.9
Work Limitations1
- 30% of adults with arthritis find stooping, bending, or kneeling very difficult.
- 20% cannot or find it very difficult to walk 3 blocks or push/pull large objects.
- People with OA (working age) experience lower employment rates than those without OA. Research suggests that arthritis-related activity limitations might contribute to their lack of employment.
Figure 22
Economic Burden
The overall economic burden associated with OA in the US is estimated at $136.8 billion annually.2 This stunning figure has more than doubled over the last decade. For perspective, the annual economic cost of arthritis surpasses that of tobacco-related health effects, cancer, and diabetes. Direct medical costs reach $65 billion annually, with annual all-cause per person direct costs reaching $11,502.2
- Because of OA, an estimated 1 million knee and hip replacements are completed each year.1
- Knee OA contributes to more than $27 billion in health care costs each year.4
- In 2013, OA was the 2nd most costly health condition treated in hospitals in the US, accounting for 4.3% of all hospitalization costs.10
- In 2013, total lost wages due to OA were $164 billion, or $4,040 less per adult with OA compared to those without OA.10
- Increased absenteeism among workers with OA is fairly well documented, with workers with OA missing an average of 2 more days per year than workers without OA. Presenteeism, or loss of productivity while on the job, is more difficult to calculate but is no less costly for workers or businesses.11
OA is associated with increased comorbidity and mortality
Twenty-five percent of Americans have two or more chronic conditions, including heart disease, stroke, diabetes, cancer, and osteoarthritis (OA). In older adults, OA is the most common condition to co-occur with other chronic conditions. A number of comorbidities and co-existing conditions often occur in patients with OA.5
Relationship between OA & Comorbidities 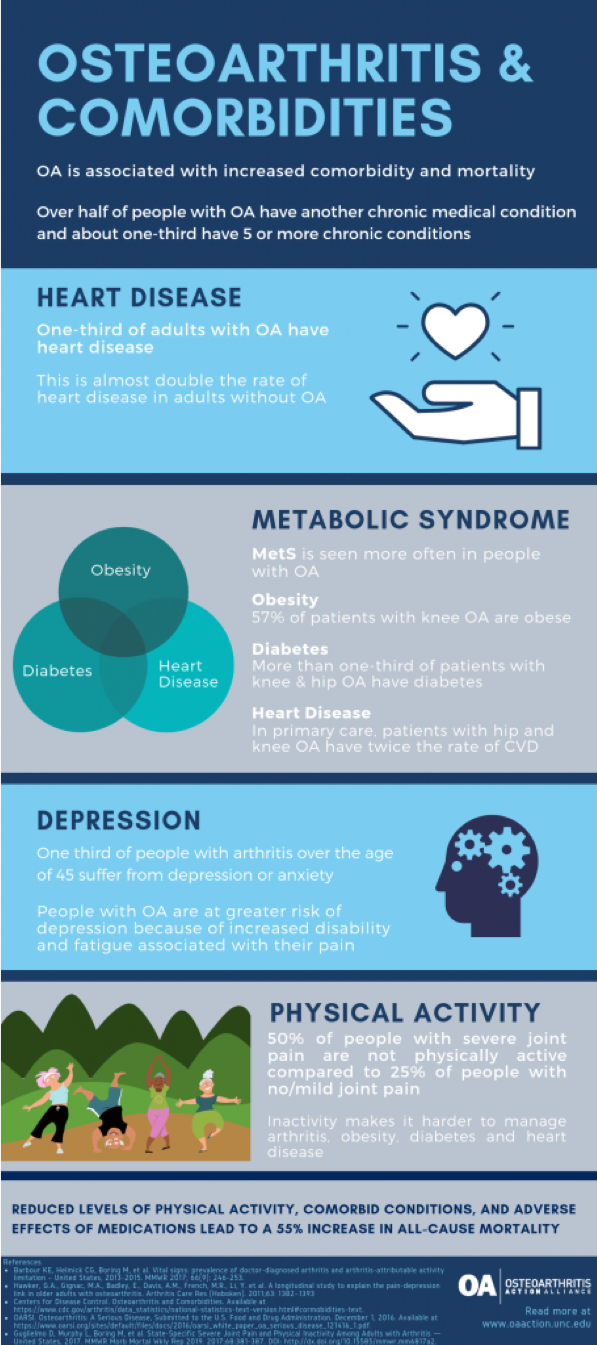
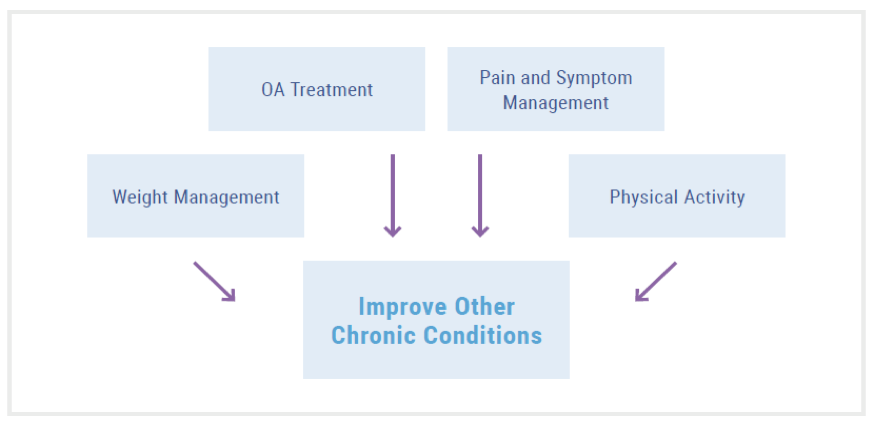
While OA is not often considered a fatal disease, studies have shown that people with OA, particularly those who are obese, are at higher risk of mortality. There are several possible explanations for people with OA having an increased risk of mortality, not the least of which is that OA is inextricably tied to other chronic conditions. Prompt and adequate management of OA can not only improve patients’ joint symptoms but may have mediating effects on patients’ other comorbid conditions as well.14,15
While advancing age, physical inactivity, and obesity likely explain the high prevalence of OA with other chronic conditions such as diabetes, hypertension, and heart disease, the relationship between OA and other comorbidities is complex.
Reduced Physical Activity
Physical inactivity is a known risk factor for most chronic conditions, including heart disease and diabetes, as well as obesity, which, in itself, is a risk factor for many chronic conditions.16 Based on the 2015 US National Health Interview Survey, the CDC found that 36.2% of adults with arthritis met the recommended weekly aerobic guideline of more than 150 minutes of moderate aerobic activity and only 17.9% met the recommended 2 days of muscle strengthening exercises per week. Compared to people without arthritis, in age-standardized terms, these rates were 10 percentage points, 6 percentage points, and 7 percentage points lower, respectively.
This study also found 75% of adults with arthritis had one other chronic condition, and the likelihood of meeting the recommended physical activity guidelines decreased as the number of comorbidities increased.17 Being physically inactive places people with OA at greater risk of heart disease, diabetes, and obesity.14
A person’s ability or desire to participate in exercise therapy (e.g., cardiac rehabilitation, regular physical activity) as a treatment option for heart disease, diabetes, or obesity may be limited as a result of OA-related pain and functional limitations.
There’s no cure, but there are strategies for disease management
While there is currently no cure for osteoarthritis, there are a number of lifestyle modifications that people can make to help ease symptoms like pain, fatigue, and swelling. The Centers for Disease Control and Prevention (CDC) recommends taking part in self-management education programs (SME), increasing physical activity levels, and managing weight. In support of these recommendations, the CDC Arthritis Program lists a number of programs that they consider arthritis-appropriate evidence-based interventions.
[CLICK HERE FOR LINK TO REFERENCES]
Updated 10/4/2020