Osteoarthritis: A Troubling Picture
As a nation, we are experiencing an under-recognized public health crisis: An epidemic of osteoarthritis (OA).
There is an urgent need to elevate OA as a national public health priority.
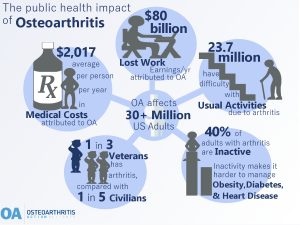
Today, 32.5 million people – 1 in almost every 7 American adults – have this serious disease that mainly affects the hands, knees, and hips. Even more alarming, OA rates are expected to increase in the years ahead as Baby Boomers age and the effects of the obesity epidemic continue to manifest. Osteoarthritis is common, expensive, and a leading cause of disability.5
Call to Action: Reducing the Burden of Osteoarthritis through Meaningful Public Policy
Osteoarthritis is widespread and costly.
Many Americans with OA face chronic pain and functional limitations, which often results in job loss and reduced quality of life. OA pain can also inhibit physical activity which interferes with the management of other chronic conditions like diabetes, heart disease, and hypertension. Our country suffers, too. It is dragged down by the social and economic costs of OA. This disease is a common cause of disability, it contributes to escalating health care spending, and it limits national productivity.
Unfortunately, OA is met with complacency.
Despite the great individual and national costs of OA, little attention is given to this disease. This is due in part to the misconceptions that arthritis causes only “mild aches and pains,” is an inevitable part of aging, and that nothing can be done to prevent or relieve it.
Yet in some cases, OA can be prevented and its consequences can be minimized.
Evidence shows that injury prevention and weight loss can prevent OA from occurring, and weight loss or maintenance, physical activity, and self-management education can reduce the symptoms and progression of OA.
 Some facts about arthritis management:
Some facts about arthritis management:
- Physical activity can reduce pain and improve physical function by approximately 40%.1
- Self-management education workshops can help reduce pain, fatigue, and depression by 10% to 20%.1
- However, only 11% had taken a self-management education workshop.1 Adults with arthritis are more likely to attend a self-management education program when it is recommended by a healthcare provider. Learn more on our Living With osteoarthritis page.
How OA Affects Individuals with the Condition
Many Americans with OA face chronic pain and functional limitations, which often results in job loss and reduced quality of life. OA can also negatively affect mood, sleep, and participation in social and leisure activities.9
- OA is a leading cause of disability: In 2010, there were approximately 17 million years lived with disability from hip and knee OA around the world.10
- In a global study of 291 conditions, hip and knee OA was ranked as the 11th highest contributor to disability.10,11
- One in four people with knee OA have pain while walking and have difficulty doing major activities of daily life such as climbing stairs, kneeling, or stooping.12
- OA is a common comorbid condition. More than half of all adults with diabetes or heart disease also have arthritis.1 Nearly one-third of adults with obesity have arthritis.
- OA limits physical activity and complicates management of other diseases. OA pain, or fear of pain, causes many people to be sedentary, even though physical activity is an important management strategy for OA and other chronic illnesses.1,13, 14
For more on the national burden of osteoarthritis and a list of references head to our page on the Cost of Osteoarthritis.
If you would like to help us shape the policy agenda of the OA Action Alliance, join us.
Updated 5/19/2022
